BLOGS
What is the difference between an osteopath, chiropractor and a physiotherapist?
Osteopathy, chiropractic, and physiotherapy are all forms of manual therapy, but they have different philosophies and approaches. While all three professions aim to improve health and function, osteopathy has a more holistic approach, chiropractic focuses on spinal health, and physiotherapy emphasises rehabilitation and movement.
1. Osteopathy
- Focuses on the whole body, emphasising the interrelationship between muscles, bones, connective tissue and organs and how fluid movement expresses itself within our anatomy.
- Osteopaths use a hands-on approach to diagnose and treat various conditions (not just musculoskeletal), often employing techniques such as stretching, massage, spinal and joint manipulation, gentle connective tissue release and cranial fluid dynamics.
- Aims to improve overall health and wellbeing, considering lifestyle and environment.
- Focus on understanding the root cause of the problem.
2. Chiropractic
- Primarily focuses on the diagnosis and treatment of musculoskeletal disorders, especially those related to the spine.
- Chiropractors use spinal adjustments and manipulations to restore alignment and improve function.
- Often emphasizes the connection between the spine and the nervous system.
3. Physiotherapy
- Addresses movement and function through rehabilitation, prevention, and education.
- Physiotherapists assess and treat physical impairments or disabilities using exercises, manual therapy, and modalities like ultrasound or electrical stimulation.
- Focuses on improving mobility, strength, and overall physical performance, often after injury or surgery.
Philosophy and Approach - Osteopathy
Osteopathy was founded in the late 19th century by Dr. Andrew Taylor Still, who emphasised a holistic approach to health. The philosophy of osteopathy is based on the belief that the body is a unit, and the interconnectedness of the body's systems is crucial for overall health. Osteopaths view the body’s structure (bones, muscles, and connective tissues) and function (physiological processes) as interrelated, and they believe that any dysfunction in one area can affect the others.
Techniques
Osteopaths use a variety of hands-on techniques, including:
- Soft Tissue Manipulation: This involves stretching the muscles to relieve tension and improve circulation.
- Joint Mobilisation: Gentle movements are used to increase the range of motion in joints.
-Fascial Release: This technique targets the fascia (connective tissue) to relieve pain and improve movement.
- “Cranial” Osteopathy: An extremely gentle but powerful form of manipulation, first discovered and practiced on the skull and cranial structures but can treat any part of the body; it relies on stimulating the body’s own ability to self-correct.
Osteopathy often incorporates lifestyle advice, such as nutrition and exercise, to promote overall health. The treatment plan may also include a focus on stress management and ergonomic adjustments.
Conditions Treated
Osteopathy can be beneficial for a wide range of conditions, including:
- Musculoskeletal pain (back pain, neck pain)
- Joint pains
- Sports injuries
- Postural issues
- Headaches and migraines
- Nerve pain (e.g. sciatica)
- Digestive disorders
- Restlessness in babies
- Symptoms caused by arthritis
Philosophy and Approach - Chiropractic
Chiropractic care originated in the late 19th century with the work of Daniel David Palmer. Chiropractors primarily focus on the diagnosis and treatment of mechanical disorders of the spine and their effects on the nervous system. The central philosophy is that spinal misalignments (subluxations) can interfere with nerve function, leading to various health issues.
Techniques
Chiropractic treatment is most commonly associated with spinal adjustments, which involve:
- Spinal Manipulation: A specific technique to realign the vertebrae, often resulting in an audible "crack." This is intended to restore normal function and alleviate pain.
- Flexion-Distraction Technique: A gentle technique that involves stretching the spine to relieve pressure on intervertebral discs.
- Soft Tissue Techniques: Chiropractors may also use massage and stretching techniques to address muscle tension and support the spinal adjustments.
Chiropractors may provide lifestyle and nutritional advice, focusing on maintaining spinal health and overall wellness.
Conditions Treated
Chiropractic care is commonly sought for:
- Back pain
- Neck pain
- Headaches
- Sciatica
- Joint issues
Philosophy and Approach - Physiotherapy
Physiotherapy, also known as physical therapy, has its roots in the rehabilitation field, emphasising the restoration of movement and function. Physiotherapists focus on the body’s ability to move and perform physical activities. Their approach is rooted in evidence-based practice, combining clinical expertise with the best available research and patient values.
Techniques
Physiotherapists employ a wide range of techniques, including:
- Therapeutic Exercise: Customised exercise programs designed to improve strength, flexibility, and coordination.
- Manual Therapy: Hands-on techniques to mobilise joints and soft tissues.
- Electrotherapy: Use of electrical modalities (e.g., ultrasound, TENS) to reduce pain and promote healing.
- Education: Providing patients with information on injury prevention, posture, and ergonomics.
Physiotherapy often involves the use of rehabilitative exercises to restore function following injury, surgery, or illness. The goal is to enable patients to regain independence and improve their quality of life.
Conditions Treated
Physiotherapy is suitable for a variety of conditions, including:
- Post-surgical rehabilitation
- Sports injuries
- Chronic pain conditions (e.g., arthritis)
- Neurological conditions (e.g., stroke)
- Respiratory issues
Key Differences
1. Focus and Philosophy:
- Osteopathy: Holistic approach focusing on the interconnection of body systems with a strong belief that the body is able to heal itself if the underlying environment can support it with good balanced movement, free of tension and restriction.
- Chiropractic: Emphasises spinal health and its relationship to the nervous system, thus enabling the whole body to be treated via the spine.
- Physiotherapy: Focuses on rehabilitation, movement, and functional recovery.
2. Techniques Used:
- Osteopathy: Involves a wide range of hands-on techniques, including soft tissue manipulation, connective tissue release, cranial osteopathy and spinal manipulation when required.
- Chiropractic: Primarily focuses on spinal adjustments and manipulations.
- Physiotherapy: Utilises therapeutic exercises, manual therapy, and electrotherapy.
3. Conditions Treated:
- Osteopathy: Treats a broad range of conditions, including back and musculoskeletal pain, headaches, digestive issues, sports injuries and the retained effects from previous trauma .
- Chiropractic: Commonly addresses spinal and musculoskeletal disorders.
- Physiotherapy: Covers rehabilitation for injuries, surgeries, and various medical conditions.
While osteopathy, chiropractic, and physiotherapy share some common ground in manual therapy, their philosophies, techniques, and areas of focus are distinct. Traditionally osteopathy is seen as a more gentle approach, Chiropractic focussed on the spine with clicking type manipulation and physiotherapy prescribing exercises for rehabilitation.
Prolapsed or "slipped" Disc
People are often told that their neck or back pain, sciatica or other nerve symptoms are due to a disc problem; there are lots of terms used such as “slipped disc”, “ruptured disc”, “herniated disc”, “prolapsed disc”, “strained disc”, “degenerative disc” or “thinning disc” but what is a disc, what is meant by “slipped” and can an osteopath help?
What is a disc?
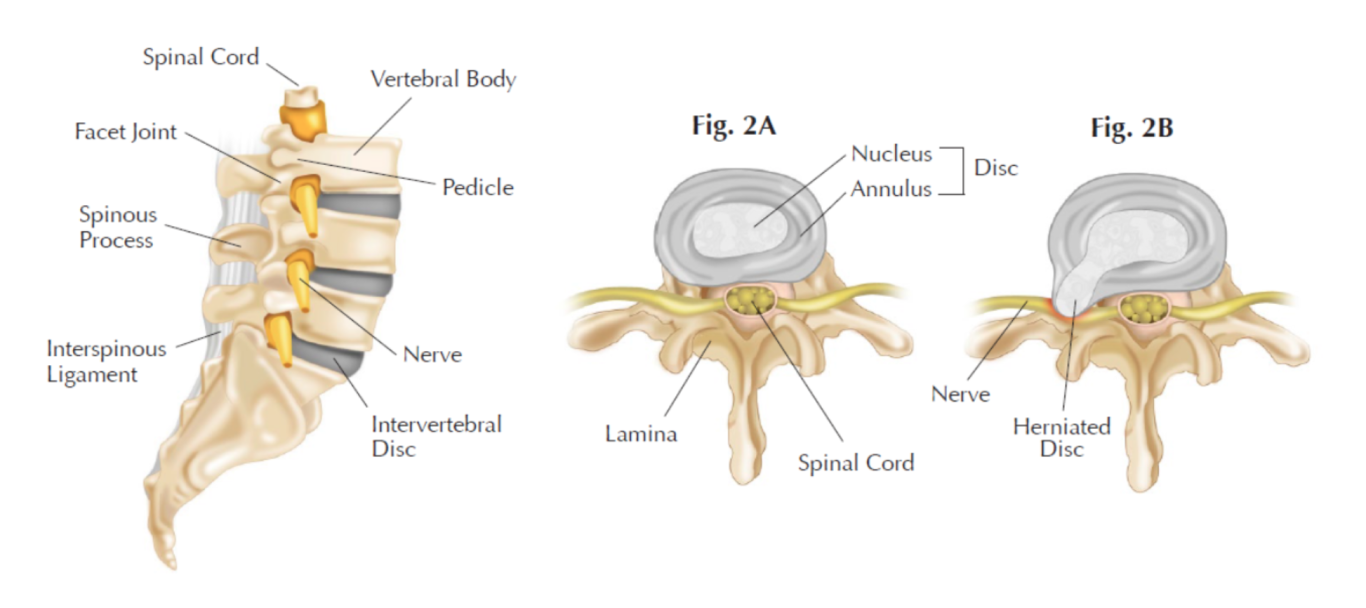
The disc is actually called an intervertebral disc – a structure found between the bony spinal vertebrae (the disc is coloured grey in the diagram above - Fig 2A is a normal disc), similar to a tyre with the tyre part being a tough fibrous outer ring (annulus) and the centre (nucleus) being gel-like. There are 23 discs in the spine. The disc acts as a shock absorber, joins the spine together and helps give the spine its curves.
What can happen to the disc?
With age and depending on activity, this shock absorbing capability reduces as the disc wears and looses height due to fluid loss. Small cracks can appear in the outer walls and, if put under undue strain, the disc can start to be pushed out of shape and bulge. If the strain on the disc continues or a one-off incident of lifting something heavy, combined with bad posture, the inside gel-like nucleus pushes through the outer walls causing what is called a disc prolapse or herniation (often nicknamed as a “slipped disc”). The whole disc does not actually slip anywhere but the gel-like centre slips through the crack in the outer ring to then form a bulge on the outside of the disc (shown above in Fig 2B).
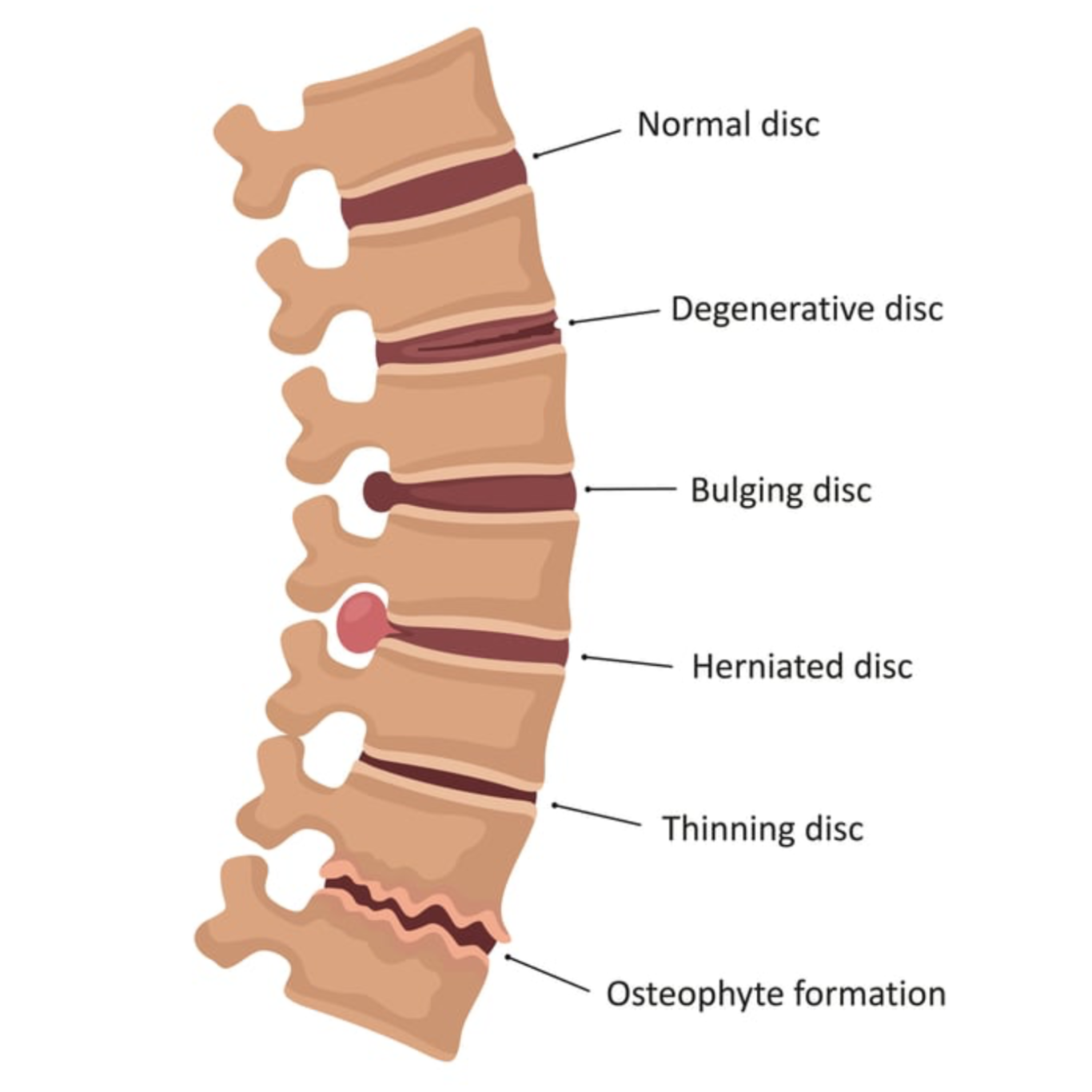
The diagram below shows different changes to the disc:
A degenerative disc can happen with normal wear and tear as we get older or with excessive pressures placed on the disc as it performs its shock absorbent function; the outer fibres of the disc tear and deteriorate reducing its ability to support the spine so efficiently. In ages 20 through to 50, this degeneration can leave the disc more prone to bulging and herniation.
A bulging disc happens as the outer ring of the disc deteriorates and its shape distorts.
A herniated disc is when the inner gel-like part of the disc passes through the damaged outer ring and solidifies as a larger bulge on the outside of the disc.
Thinning disc: as we get older our tissues tend to dehydrate and this can result in a disc becoming thinner; it can also be a sign of previous injury or increased pressure being placed on the spine e.g. heavy lifting.
Degenerative disc with osteophyte formation: osteophytes are bony spurs which form on the bony margins and are a common feature of “wear and tear” osteoarthritis. This leads to stiffness and discomfort.
Complications of this disc prolapse
This will depend on the severity of the prolapse and exactly which direction it has gone in:
If it is a small bulge then the person may not experience any symptoms at all or a localised discomfort as the bulge presses on the connective tissues which surround the spine.
If it is more severe it can press on the nerves of the spine causing tingling, numbness, pain or power loss in the arms or legs depending on whether the problem is in the neck or low back.
In a few cases, very severe prolapses can press on the spinal cord causing compression which requires urgent medical attention ( called caudal equine syndrome). Whenever a patient presents to an osteopath with possible disc and/or nerve problems, the osteopath is trained to ask appropriate questions and perform some basic tests to recognise if there is anything more severe going on and then act accordingly, referring as necessary.
Symptoms of disc prolapse
Symptoms are caused by the bulge putting pressure on the various structures around it and can be quite varied; the bulge/prolapse tends to extend into the space where the spinal nerve exits from and this can cause pressure on the nerve. The gel-like nucleus also contains inflammatory proteins which can also irritate the nerve.
Symptoms can include:
Lower back pain
Numbness or tingling in your shoulders, back, arms, hands, legs or feet
Neck pain
Problems bending or straightening your back
Muscle weakness
Pain in the buttocks, hips or legs
Sciatica
Standing, sitting, walking, sneezing, coughing and bowel movements can all be difficult.
All these symptoms can be caused by other problems which are not disc-related (some less severe musculo-skeletal reasons and some more severe). This is why accurate diagnosis is very important; as an allied health professional, an osteopath is fully trained to help patients in this diagnosis and discuss any need for further investigation or referral.
Treating the prolapsed disc
Whether it is a small bulge, minor strain or prolapse, the disc has sustained physical damage which requires time to resolve and repair. Osteopaths encourage this repair by identifying why that particular disc was the one that had the problem in the first place (possibly trauma or wear and tear for example) and then treating to ensure that the spine is optimally placed to enable healing and the protective spasm around the problematic disc is eased. Advice as to how to manage the problem will also be given to the patient including postural tips, the use of hot or cold packs and stretching as appropriate.
The traditional medical approach to a disc problem is often to offer a combination of painkillers, anti-inflammatories and possibly muscle relaxants which can work in conjunction with osteopathic treatment to resolve the disc problem more speedily. If the problem persists or there are any worrying symptoms, the patient can be referred back to their GP for further investigations and, as a last resort, onto a specialist for spinal injections and/or an operation if required.
How does the disc heal?
A recent study in 2017 showed that at least 66% of disc prolapses resolve with conservative treatment - that means with no surgery. It is generally said that a prolapsed disc can take 6 - 12 months to heal.
There has been a lot of debate over the years as to whether a prolapsed disc actually can reabsorb; certainly it is very unlikely that the fluid will return to the gel-like nucleus, the damage in the outer ring completely heal and all return to as it was before but there is plenty of evidence to show that there can be partial reabsorption and the bulge/herniation can become smaller.
How does this happen?
An immune response by your body. Sometimes your body recognizes the portion of the disc that has herniated as foreign material and attacks it, reducing the fragment in size and removing its inflammatory proteins.
Absorption of water. The herniated fragment of the disc contains water. Over time this water will be absorbed by the body, causing the herniated segment to shrink in size. As it shrinks it may no longer affect the nearby nerve.
Mechanics of the spine. Through manual treatment such as osteopathy and exercises, the symptomatic portion of the disc can be moved inward toward the disc and away from the spinal nerves. Osteopathic manipulation improves the mobility of the structures around the disc, fluid movements become more efficient which leads to an improved healing response.
As symptoms are cause by the disc bulge putting pressure on the connective tissue or spinal nerve, a small reduction of size of the bulge or an improvement in spinal mechanics can lead to a marked reduction/resolution of symptoms. As MRI scans are much more commonly used nowadays, it has been shown that many people have a bulging or prolapsed disc but without symptoms, often from a trauma years ago; in fact, there are times when they had never had any back problems and were having a scan for a completely different reason.
What this shows is that why people get symptoms is a down to a more complex set of reasons; the body always wants to be well (homeostasis) and will do whatever it can to adapt and compensate to the strains and damage placed on it. A small amount of change of size/pressure/fluid adaptability regarding the disc can lead to a marked reduction of symptoms or even full resolution.
Osteopaths treat the whole body increasing overall mobility, balance and integration of fluids dynamics to create the optimum foundation for healing, fluid absorption, spinal alignment and immune response. It is always worth a phone call to see how we might be able to help - our osteopaths can always offer a free 15 minute chat to discuss things in more detail: 01225 967630 or email parkfieldosteopaths@aol.com
©Copyright. All rights reserved.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.
